Hashimoto’s thyroiditis and hypothyroidism are two serious thyroid disorders shrouded in mystery.
While standard treatments like levothyroxine aim to replace missing thyroid hormones only, millions continue to suffer lingering symptoms of autoimmune diseases.
But what if there were an underground solution that could calm the autoimmune disease fire fueling thyroid damage?
Low Dose Naltrexone or LDN is a little-known immune system modulator that could change the way we approach Hashimoto’s thyroiditis (and many other autoimmune disorders) and hypothyroidism—if given the chance.

At ultra-low doses (that we’ll outline below), the generic drug naltrexone may calm the autoimmune response, rebalance autoimmune processes, and relieve chronic health issues where all else has failed for those with autoimmune diseases.
Some integrative doctors have started using low dose naltrexone off-label to manage Hashimoto’s thyroiditis and support thyroid health—with promising reports from many patients of reduced pain, improved mood and mental clarity, sustainable weight gain and loss, and even the ability to lower or stop other medications under medical guidance.
However, low dose naltrexone remains outside the mainstream and is not FDA approved for thyroid conditions, leaving many to write it off as another wellness fad.
That’s why we’re going to answer some important questions:
- Why are most physicians unaware of low dose naltrexone ‘s potential?
- Does evidence from clinical studies really support its use for autoimmune conditions (mainly Hashimoto’s thyroiditis) and hypothyroidism?
- How does low dose naltrexone interact, if at all, with traditional thyroid hormone treatments?
- What is the appropriate dosing protocol, and how soon might someone on thyroid regimen expect to feel low dose naltrexone ‘s benefits for their autoimmune condition?
- Can LDN replace thyroid hormone replacement therapy?
For those with thyroid disorders beyond Hashimoto’s thyroiditis struggling to calm lasting symptoms, having answers to these questions could mean the difference between persistent suffering and a hope finally realized.
In this comprehensive resource, you’ll discover exactly what low dose naltrexone is, how it works to temper autoimmune disease responses and restore function, and the scientific evidence both for and against using low dose naltrexone for Hashimoto’s thyroiditis and hypothyroidism.
We’ll discuss how low dose naltrexone and thyroid medications may interact, optimal dosing for success, and additional diet and lifestyle measures critical to calming chronic inflammation and supporting thyroid health from all angles.
By article’s end, you’ll have the knowledge you need to make an informed decision and craft a personalized recovery plan equipped to address the root causes sustaining your autoimmune condition.
The power to reclaim wellness is within your grasp—if you choose to reach for it in your thyroid journey.
Are you ready to take the first step on an unexpected thyroid journey towards health?
What is Low Dose Naltrexone?
Let’s first discuss Naltrexone… because as you would guess, low dose naltrexone is just a smaller amount of naltrexone (shocking revelation).
Naltrexone is an FDA-approved drug initially used to treat opioid addiction and alcohol use disorder.
At high doses of 50 to 100 milligrams, naltrexone blocks opioid receptors in the brain that trigger a response to substances like morphine or alcohol.

However, at very low doses of just 3 to 4.5 milligrams, naltrexone exhibits an unexpected anti-inflammatory properties and immunomodulating effect—a discovery that could have major implications for managing autoimmune diseases like Hashimoto’s thyroiditis.
How Low Dose Naltrexone Affects Autoimmune Diseases
The anti-inflammatory properties of low dose naltrexone (LDN) can be attributed to its temporary blockade of opioid receptors, which are present throughout the body’s cells, including immune cells (Toljan & Vrooman, 2018). According to Toljan and Vrooman (2018), “LDN leads to a temporary and reversible increase in endogenous opioids, especially OGF and met-enkephalin.”

Endorphins are also capable of regulating an overactive immune system (Smith, 2007). By triggering short-lived disruptions and decreasing inflammation in the opioid system, LDN may lead to long-term balance in the immune response (Brown, 2017, Sacerdote 2008).
In autoimmune diseases like Hashimoto’s thyroiditis, the immune system mistakenly targets the body’s own tissues. LDN could help reign in these confused immune system responses through several mechanisms:
Endorphins released in response to LDN bind to receptors on immune cells and may reduce inflammation by decreasing inflammatory cytokine concentration (these are inflammatory proteins) (Sharafaddinzadeh 2010).
Lowering chronic inflammation can help calm autoimmune processes. Repeated short-term inflammatory responses to LDN lead to more decreasing inflammatory cytokine concentration over time for long-term anti-inflammatory effects (Brown, 2018).
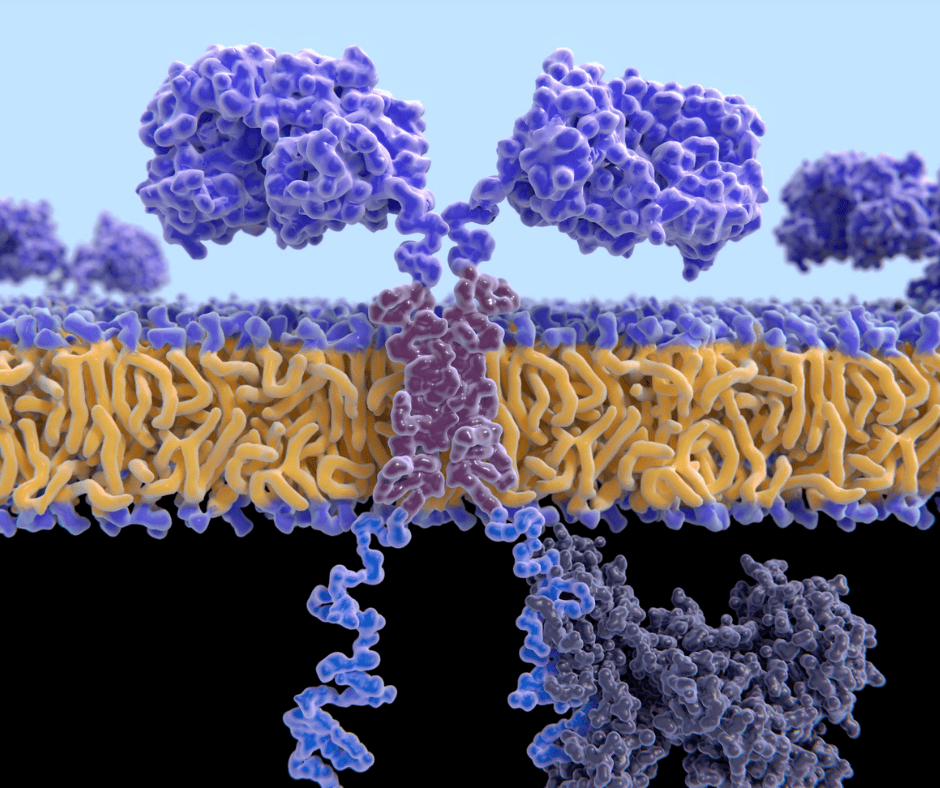
By blocking opioid receptors temporarily, LDN makes immune cells more sensitive to the effects of endorphins over time (Younger 2014).
LDN also calms down an excessive immune system response by promoting more anti-inflammatory immune cells (Toljan 2018)
In other words, LDN helps by promoting immune cell regulation that can help curb autoimmunity.
However, if you’ve been around the “science block” you would know how many times a mechanism looks great “on paper” but doesn’t pan out in the real world.
So, how has LDN done for autoimmune diseases in the research?
What the Research Says About LDN for Autoimmune Diseases
Multiple Sclerosis
Gironi et al. (2008) conducted a pilot trial of LDN in primary progressive multiple sclerosis and found that “LDN was safe and well tolerated, and some of the patients experienced a clinically meaningful improvement.”
This suggests that the blockade of opioid receptors for several hours following each dose elicits a mild response that promotes the production of endorphins—neurotransmitters responsible for inducing feelings of well-being and providing soothing and analgesic effects.
Fibromyalgia
In a pilot study of fibromyalgia patients, Younger and Mackey (2009) reported that “the medication was associated with a significant 30% reduction in daily pain.” This further supports the notion that LDN has a beneficial impact on various autoimmune and inflammatory conditions through its modulation of endorphin production.
Crohn’s disease
Two studies (one in adults and the other in kids) with 46 participants total assessed the efficacy and safety of low-dose naltrexone (LDN) in treating active Crohn’s disease (Parker 2018).
The adult study found no significant difference in clinical remission between LDN and placebo, but a significantly higher clinical response and endoscopic response were observed in the LDN group.
In plain English, LDN appears to reduce symptoms and signs of Crohn’s but did not lead to full-on remission.
The pediatric study reported that 25% of LDN-treated patients achieved clinical remission compared to none in the placebo group.
No serious adverse events were reported in either study, and pooled data showed no statistically significant differences in adverse events.
Rheumatoid arthritis
A study looked at 360 patients’ prescriptions one year before and after starting LDN in 2013 (Raknes 2019).
What they found was quite promising!
Among those who consistently used LDN, there was a 13% reduction in overall medicine usage (about 73.3 fewer defined daily doses per patient) and a 23% drop in analgesic usage (21.6 fewer doses). They also observed fewer users of NSAIDs, opioids, DMARDs, and TNF-α antagonists in this group. However, these benefits weren’t seen in patients with lower LDN exposure.
So, LDN has shown some effect for autoimmune conditions… but what about Hashimoto’s?
The Case for Using LDN for Hashimoto’s and Hypothyroidism
So, LDN seems to be effective for other autoimmune conditions…
Before we dive into the research findings and pull from the stories of others…
I have a shocking statement for you.
All the other autoimmune conditions we talked about above and Hashimoto’s are… different!
(That should not have been a revelation)
So, let’s break down how LDN may be helpful for Hashimoto’s
How LDN may support your thyroid gland, thyroid hormone function, and production
Interestingly LDN may affect thyroid function for Hashimoto’s as an autoimmune thyroid disease and non-autoimmune hypothyroidism alike.
There was this study by Vuong et al. (2010) reviewed the effects of opioids and endorphins on thyroid hormone.
I’ll keep it simple here.
Opioids often increase TSH in humans… but also have been shown to decrease it in humans.
Endorphins lead to a decrease in TSH as well.
Now, the paper summarizes many (many) papers, but your main take-away is that these substances directly affect the secretion of TSH that would impact your thyroid downstream.
More important to note, there is no crystal clear relationship between thyroid function and the same system LDN uses to work its magic with the other autoimmune conditions we mentioned above.

So, how do these mechanisms work out in the real world for those with Hashimoto’s?
So what does the research show?
So there is one published research study on hashimoto’s and LDN use that I was able to find in 3 hours of searching around.
(I’m basically double-certified in finding information online; Google asks me for help sometimes).
This study was performed by the same folks who brought us the same study on rheumatoid arthritis.
Using a similar methodology, they found that Hashimoto patients taking LDN did not change how much thyroid medication they got (Raknes, 2020).
Now, this evidence is not particularly compelling.
Literally, the finding was that people who took LDN did not get fewer thyroid medications.
No mention of thyroid markers, symptoms, etc.
At this point I would like to remind you that “absence of evidence is not evidence of absence”
That is, this research doesn’t answer our primary question of “does LDN help for hashimoto’s?” either way
So, we are forced to turn to anecdotal evidence…
Anecdotal Evidence
The majority of anecdotal evidence comes from pharmacist Isabella Wentz. Here’s two anecdotes/stories.
LDN and Improved Thyroid Function
In her book “Hashimoto’s Protocol,” Dr. Isabella Wentz shares the story of a patient named Julia who was struggling with Hashimoto’s disease, an autoimmune thyroid condition.
Julia experienced a range of symptoms, including fatigue, weight gain, and depression. Despite trying conventional treatments, her thyroid function did not improve, and she continued to feel unwell.
After researching alternative treatments, Julia learned about LDN and decided to discuss it with her healthcare provider. After getting approval, she started taking LDN as part of her treatment plan.
Over several months, Julia noticed a significant improvement in her symptoms. She experienced increased energy, gradual weight loss, and a lifting of her depression. Additionally, her thyroid function tests showed improvement, indicating that the LDN was positively affecting her immune system and thyroid function.
LDN and Reduced Thyroid Antibodies
Another anecdotal story comes from a woman named Karen, who shared her experience with LDN and Hashimoto’s disease on a health forum.
After hearing about LDN’s potential benefits for autoimmune conditions, Karen discussed it with her doctor and decided to give it a try.
Within a few months of starting LDN, she noticed that her hair loss had slowed down, her joint pain had reduced, and her mental clarity had improved. Moreover, her thyroid antibody levels dropped significantly, indicating a reduction in autoimmune activity. Karen continued to take LDN as part of her ongoing treatment plan, and she felt that it played a crucial role in her overall improvement.
Anecdotal evidence is just that… a story.
Yes, it may be possible but don’t hang your hat on it as “proof” for any means here.
Now, just because there is limited evidence for or against LDN for Hashimoto’s doesn’t mean hashimoto’s patients can’t get other benefits.
LDN benefits for Hashimoto’s and hypothyroid patients
LDN offers much sought-after perks for the Hashimoto’s and hypothyroid set. A motley crew of tired, achy, brain fogged and weight gain or loss resistant patients may finally have cause to celebrate.
At the top of the list promising treatment, is fatigue fleeing in the face of LDN’s energy boosting effects. Several studies report improved vitality in patients on LDN for other autoimmune conditions in the studies we’ve mentioned above.
Hashimoto’s patients are also prone to pain from inflammation and muscle spasms that readily respond to LDN’s pain-relieving effects.
Mood and cognition, frequent casualties of Hashimoto’s and hypothyroidism, may experience a turnaround on LDN as well. Patients report improved memory, focus and an end to brain fog within weeks to months of starting LDN. (This may also have a big benefit of multiple sclerosis as well due to the nervous system involvement.)

Its stimulatory effects on dopamine and other feel-good neurotransmitters could lighten depression and lift darkened moods. Patients may reclaim their quick wit and sharp memory, no longer blaming Hashimoto’s for every stray thought lost or word on the tip of their tongue.
While LDN is no panacea, for those struggling with Hashimoto’s and hypothyroid symptoms despite conventional treatment, a bit of respite may await the patient brave enough to try. Life’s pleasures return one by one—energy to burn, pain-free days, mood and mind restored, favorite jeans buttoning once more. LDN deserves a toast for giving some semblance of normal life back to those who feared it had ended.
But, like with anything in life, you need to consider the side effects and risks of LDN.
Safety, side effects, and risks of LDN
While touting benefits galore, LDN does come with a few health warnings worth noting. At doses of just 3-4.5mg, LDN is considered extremely safe with minimal risks or side effects for most.
However, some may experience nausea, digestive upset, vivid dreams or headache when first starting that typically pass. Unlike high dose naltrexone, LDN is nontoxic and unlikely to cause damage to the liver, kidneys or other organs even with long term use.

That said, a select few may face trouble in LDN paradise. Those with a history of opioid use disorder should avoid LDN as it could trigger temporary withdrawal symptoms by blocking opioid receptors. For a clever fellow, this seems an obvious concern best discussed with your doctor before trialing LDN.
While not common, certain medications like opioid painkillers, benzodiazepines for anxiety or sleep disturbances and medical marijuana may negate LDN’s effects or cause side effects when combined.
Check with pharmacists for interactions and schedule doses to avoid overlap. A bit of timing and coordination may allow diverse treatments to play nicely together.
For a sparse minority, mood-related side effects like anxiety, irritability or depression may surface on LDN. If your mental state takes a turn for the worse after starting LDN, discuss with your doctor promptly about changing the dosage or stopping the medication.

As increased endorphin function and neurotransmitter fluctuation come with LDN use, temporary dips in mood are possible but sustained changes warrant attention.
Particularly during initiation or dosage increases, some experience transient insomnia or sleep disturbances on LDN’s erratic wave of stimulation and adjustment.
An afternoon dose and timing adjustments may help most sleep through the night. For persistent sleeplessness, a brief med holiday or dose reduction could provide relief without losing benefits.
While larger controlled clinical trials would seal the deal, LDN’s safety record gleaned over 30 years of use and study suggests benefits outweigh potential risks for most when used responsibly under medical guidance.
Start low and go slow is the mantra, with patience through temporary discomfort knowing improvements often await on the other side. Look out for the rare few unable to tolerate this wonder drug—but odds are good the vast majority will do just fine.
Now, why don’t most doctors and I advocate for LDN???

Why most doctors don’t prescribe LDN
While LDN flaunts an admirable safety profile and therapeutic potential, most doctors remain unenlightened and unpersuaded of its merits.
Chalk it up to a lack of drug company-sponsored education on off-label use or skepticism of claims not backed by large-scale clinical trials — either way, LDN gets a cold shoulder from mainstream medicine.
Doctors suffer no shortage of pharmaceutical suitors flooding their offices with promises of pills for every ill. But for orphans like LDN, abandoned patentless molecules of little commercial value, the education of physicians remains barebones.
Without financial incentives or pushy drug reps extolling LDN’s virtues, doctors see no compelling reason to dust off long-held assumptions that naltrexone only numbs receptors at high doses.
While thousands of patients and over 30 countries endorse LDN for pain, autoimmune diseases, and autoimmune disorders, most doctors balk at the lack of ironclad evidence from large controlled trials.
Anecdotes and case studies make for interesting tales but fall short of the rigorous proof required to change clinical practice. And without FDA approval for specific autoimmune disease conditions yet, insurance coverage remains limited and liability a concern. Why switch from standard treatments and venture into legally murky waters?
Forces far more complex than health outcomes alone steer the medicine we practice. Doctors have little choice but follow guidelines shaped by clinical trials funded by for-profit companies with money to gain.

While patients pine for lower-cost options with fewer side effects, if data to support them never emerges and all education comes from competitors’ products, change comes slowly if at all.
The tragedy is that many patients with cancer therapy might benefit now if given the chance, await evidence and approval promising treatment that may come too late or never at all due to lack of commercial incentive.
Patients suffering failed to respond to accepted treatments are left out in the cold with few low-risk options. Doctors wishing to help have their hands tied needing to follow the standard of care.
So the impasse remains — an inexpensive generic drug of striking promise garners dust, doctors stay the course, and patients suffer, all for lack of money changing hands.

A sad statement about modern medicine indeed. But for a dedicated few pioneering doctors, and patients willing to take a calculated risk, LDN still finds open minds and gets the chance to work wonders.
But… I know you.
You’re literally searching on the internet right now.
So let’s talk about how to find a doctor that knows about LDN.
How to find a doctor willing to prescribe LDN
So you’ve heard the whispers of low-dose naltrexone working wonders and want to give this underdog drug a chance. The only catch is, how to find a doctor that will prescribe LDN?

The quest to secure the low dose naltrexone coveted by so many waiting patients may require patience and a nose for open-minded doctors thirsting for a better way.
A good place to start is the LDN Research Trust’s directory of over 1500 LDN-friendly physicians worldwide. Search by location and view contact details to find doctors prescribing for a range of conditions.
Many listed have experience using LDN as an adjunct or alternative to other treatments. If lacking options nearby, don’t lose hope — telephone consultations with listed physicians are also possible and can result in LDN shipped directly to your local pharmacy.

Check with pharmacists in your area as well — some keep records of doctors calling in LDN prescriptions and may provide leads.
Explain you’re looking for physicians open to prescribing off-label use of a FDA approved medication with minimal risk. While unable to freely name doctors, a helpful pharmacist may point you in the right direction.
Scour integrative and functional medicine clinics which tend to be more open-minded about off-label use and alternatives to standard care.
Explain your condition and symptoms, desire to try LDN, and ask whether any doctors feel comfortable prescribing if the benefits outweigh the risks.
Some operate via monthly membership fees but seeing an integrative or functional medicine doctor such-minded practitioner even once may open access to LDN.
Private social media groups focused on your specific condition using search terms like “LDN” and “low dose naltrexone” often contain posts praising doctors providing LDN. Reach out to members noting success to ask about their prescribing physicians.
But proceed with caution in sharing private details in such forums and research any leads further.
For the brave few willing to take matters into their own hands, purchase LDN from licensed compounding pharmacies that ship direct to customers world-wide.

While legally dubious if not prescribed by a doctor, some obtain relief when all else has failed and options are few. But of course, this course of action is not officially recommended and is taken at your own risk.
When doors slam shut to an inexpensive, low-risk option that may offer relief, it’s no wonder the determined few forge their own path to access.
If the benefits of LDN seem worth the effort, stay the course. With enough poking around, the right physician match may surface — one willing to veil you in LDN’s healing grace at long last.
But, before you take that step, you need to ask yourself “how does LDN interact with any thyroid drugs I’m taking right now?”
Does LDN Interact or Interfere with Thyroid Medication?
Interactions between LDN and thyroid medications
While LDN plays nice with most, it has not yet been researched what the interaction between LDN and common thyroid medications like levothyroxine are.
As such, it is important to be cautious and gradual with this medication as your LDN aware practitioner advises.
One common practice is, starting LDN 4 hours apart from thyroid meds, then slowly inching closer as tolerated under medical guidance, allows benefits of both without upset.
Another important practice is to closely monitor your thyroid markers during use of LDN.

With proper precautions in place and the right practitioner guiding these med mixers, LDN and thyroid mediations can play nicely.
LDN may Allow Some Patients to reduce thyroid hormone replacement therapy
Yes, some patients are able to lower or stop thyroid meds under medical guidance over time, be cautioned not all will achieve this goal.
(But, do not PUSH for this to happen… this may bit you in the but/thyroid)
While LDN aims to support and improve thyroid function and health, not all achieve freedom from an underactive thyroid. For some, thyroid med needs stay steadfast or even increase to counter LDN’s effects.
Under medical guidance, decreasing thyroid meds in small increments with close monitoring of symptoms and levels is key.
Move slowly, one change at a time, rechecking at least 6 to 8 weeks apart. (Because rocking the med boat too quickly leaves everyone sea sick!)
For the lucky ones prescribed LDN able to sustain drops, lower in baby steps of no more than 25% at a time. Pushing farther faster risks a hypothyroid crash—no benefit comes from that!
For others prescribed LDN, staying the course on the same trusted doses may prove best. Either outcome counts as a win if thyroid health and wellbeing are supported.

(Turns out, it really IS about the journey, not the destination!)
Focusing on how you feel along the way rather than an endpoint sought keeps expectations in check and disappointment at bay.
The right support and mindset can make all the difference in how this med dance unfolds for you. Just keep moving with the beat that’s true!
Now, let’s discuss what a typical protocol looks like.
Dosing Protocol for LDN and Hashimoto’s
For Hashimoto’s, the LDN treatment dosing sweet spot may require a bit of trial and error.
This is for informational purposes only! This is a protocol that is common amongst people with a licensed prescriber using LDN.
This protocol is not medical advice and it is not FDA approved.
Again, here’s a typical protocol for informational purposes only

- The starting dose for most is just 1.5mg— Going low and slow prevents upset. At this starting dose, LDN is unlikely to cause side effects but may provide benefit for some.
- Many increase to 3 mg after 4 to 6 weeks if tolerated—Most will stay here for 2 to 3 months before increasing further. Patience pays off! Rushing risks rocking your med boat.
- 4.5mg is the max dose for most —Higher offers no added benefit for Hashimoto’s and may actually cause side effects for some.
- Adjustments are usually made by no more than 1.5mg at a time— Moving up or down in small increments of 0.5 to 1 mg. This isn’t a race to the finish for most.
- Many allow 8 weeks between increases— Giving your system time to adjust and any side effects to resolve before upping the dose.
- Thyroid levels are often checked 4 to 6 weeks after each increase—To ensure levels remain stable or even improve before upping the dose for most.
- Once stable dose and symptom relief are achieved, usually around 4.5mg, there’s no need to increase further for most —Recheck levels in 3 to 6 months.
- For some, the doctor may then start lowering the thyroid med—BUT only under close guidance and very slowly, decreasing by 25% or less at a time.
With the proper med pacing and close monitoring in place, LDN treatment for Hashimoto’s may prove helpful for many in lowering inflammation, stabilizing hormone levels and even slightly dropping thyroid meds.
But proceed cautiously, increasing the lowest dose that provides benefit for each person.
Now, that’s the dose… but what kind of form?
LDN in liquid or tablet form?
LDN comes in liquid or tablet form. Liquids from compounding pharmacies provide flexibility in dosing but some dislike the taste.
(Who wants cough syrup flashbacks!)

Tablets dissolve under the tongue but may irritate mouth sores or teeth.
Tablets ensure precise dosing and bypass the GI tract but for some, sublingual use causes irritation or the tablet doesn’t fully dissolve, requiring swallowing any remaining pieces.
Liquids in theory offer improved absorption but depending on the base used, the actual amount of naltrexone absorbed can vary.
There’s no “best” option, only what works for you. (Picky, picky!)

Both provide benefits so you can’t go wrong either way. The formula fitting your needs and lifestyle is the right choice. Unless the cost differential makes choice a necessity, sample both to see which you prefer.
When is the best time to take LDN?
LDN works best taken at night before bed on an empty stomach. Studies show LDN leads to increased endorphin function at night, improving sleep and easing pain.
Taking at night also bypasses daytime endorphin fluctuations and side effects are less likely when sleeping.
An empty stomach provides the ideal absorption with nothing to block uptake or compete for resources.
(No more midnight ice cream unfortunately… but maybe that’s for the better…)
Nighttime dosing yields the highest, steadiest blood levels as you slumber the hours away.
For some, a bedtime dose disrupts sleep initially so starting on a day off allows adjusting to any stimulation effects.

But for most, nighttime LDN leads to improved rest over weeks of use.
Managing side effects when starting LDN
LDN side effects are usually transient but uncomfortable.
Common culprits include vivid dreams, insomnia, nausea. (As if life didn’t give you enough stress hormones, here are some more!) Starting at a lower dose and titrating up slowly helps minimize upset.
But when side effects strike, all’s not lost.
Vivid dreams should subside quickly. Insomnia improves once adjusted but melatonin or meditation helps until then. Nausea responds to ginger, peppermint or lower dose.

(Cancel that seasickness remedy…you’re not sailing the rocky med seas just yet!)
Most side effects pass in 2 to 4 weeks. But if problematic or persistent, talk to your doctor about adjusting the dose or timing.
No need to suffer through needlessly!
(Some med dances just require a few missteps before the right rhythm is found.)
Staying hydrated, fed and rested aids adjustment to any new med. So make self-care a priority when starting LDN…your belly and your med brain will thank you!

(And a happy belly and brain make for a happy you!)
Ongoing lab testing while on LDN
LDN aims to balance what’s gone awry, so ongoing labs help gauge progress.
Check TSH, free T3/T4, thyroid antibodies every 6-12 weeks when first starting LDN or changing doses. Monitor inflammation via ESR, CRP and vitamin D, B12 levels which often need support.
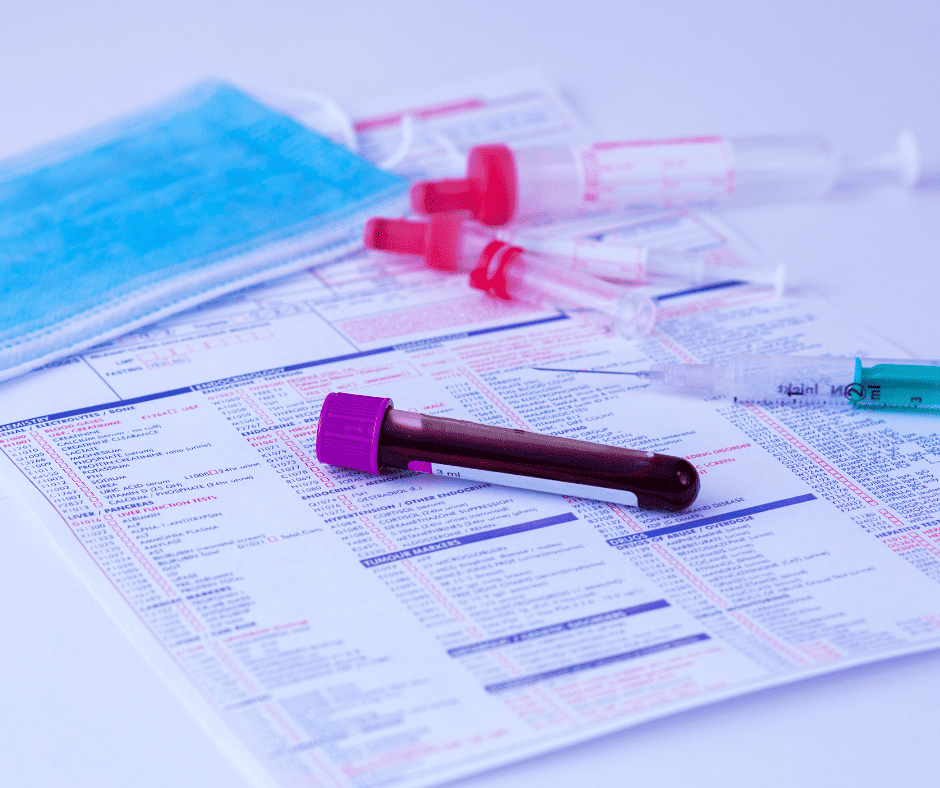
While some levels may fluctuate initially before stabilizing, significant or persistent changes warrant discussion with your doctor.
(No need to make a lab rat of yourself with excessive testing!)
But keeping a baseline and rechecking periodically provides reassurance of proper med pacing and catches imbalance early.
Celebrate positive trends but avoid judging labs alone—how you feel matters most. LDN success means improved wellbeing, quality of life.
Labs lend objective insight but the ultimate goal of a balanced body and mind can’t be measured solely by numbers on a page.
(Unless of course you’re a cyborg…then by all means, live and die by the labs!)
For the human in you, find what testing cadence provides comfort without fixation. With the right practitioner overseeing your LDN journey and ongoing progress, lab worry may wane, freeing focus to living well.
Next Steps
LDN shows promise for dampening Hashimoto’s disease activity and supporting thyroid health by reducing inflammation and balancing the immune system.
For many patients, LDN provides relief from symptoms and stabilizes hormone levels, allowing small drops in thyroid medication under medical guidance.
While LDN addresses what has gone awry in the autoimmune process of Hashimoto’s, the root cause of autoimmune condition lies deeper.
Mitochondria, our cellular energy centers, are instrumental in powering thyroid hormones and immune function. When mitochondria are struggling, hormone and immune balance soon follow suit.
Supporting mitochondria in those with Hashimoto’s is key to achieving wellness beyond symptom relief.
Simply put, you must heal your mitochondria to heal your thyroid and immune system attacks and health for the long run.
(And who doesn’t want sustainable solutions to autoimmune conditions over band-aids!)
LDN offers a starting point by dampening autoimmunity, but mitochondrial support provides the foundation for deeper healing.
Diet, lifestyle changes, targeted nutrients, and reducing environmental stressors are all required to bring mitochondria, and thus your health, back into balance. Treating the terrain—that is, the state of your body and its cellular health—rather than chasing ever-changing autoimmune symptoms is the means to lasting equilibrium.
(Time to get off the med-go-round and support what fuels your health or lack thereof: your mighty mitochondria!)
Rather than judge your progress by lab tests alone, tune into how you feel with mitochondrial and LDN support in place. Improved energy, mood and cognition, relief from chronic pain, better sleep, and an overall sense of vitality and wellbeing signal you’re on the path to remission and health regained.
While LDN may get you started, you must learn about and heal your mitochondria to complete the journey.
We invite you to join our free masterclass to discover a comprehensive plan for healing your Hashimoto’s by supporting your mitochondria.
Because your thyroid health starts where true health and immunity begin: in your cellular powerhouses that fuel your every function and form the essence of your energy and being. Your mitochondria hold the key to health reclaimed—it’s time to turn that key!
So, make sure to watch our free masterclass here → OptimalCircadianHealth.com/class
Your mitochondria will be glad you did! (And so will that little gland struggling to keep up…)

Written By: Dylan Petkus, MD, MPH, MS
Dr. Dylan Petkus is on a mission to help people overcome their health issues like sleep apnea so they are not limited by their condition or trapped by options that don’t provide full resolution.
He earned his Master’s of Science in Physiology at Pennsylvania State University where he was awarded a research fellowship and was a peer-reviewed published author. He went on to earn both his Master’s in Public Health and Medical Degree from the University of Miami Miller School of Medicine. Thereafter, he specialized in Family Medicine to help patients on the front-line of chronic disease.
Having overcome his own health challenges, including sleep apnea, he strives to help empower others to live fuller, healthier lives.
References
- Gironi, M., Martinelli-Boneschi, F., Sacerdote, P., Solaro, C., Zaffaroni, M., Cavarretta, R., … & Furlan, R. (2008). A pilot trial of low-dose naltrexone in primary progressive multiple sclerosis. Multiple Sclerosis Journal, 14(8), 1076-1083. DOI: 10.1177/1352458508095828
- Toljan, K., & Vrooman, B. (2018). Low-dose naltrexone (LDN)—review of therapeutic utilization. Medical Sciences, 6(4), 82. DOI: 10.3390/medsci6040082
- Younger, J., & Mackey, S. (2009). Fibromyalgia symptoms are reduced by low-dose naltrexone: A pilot study. Pain Medicine, 10(4), 663-672. DOI: 10.1111/j.1526-4637.2009.00613.x
- Brown ES, et al. Low-dose naltrexone for disease prevention and quality of life: Effects on inflammation, oxidative stress, and depression. Am J Hosp Palliat Med. 2018;35(1):114‐118. https://pubmed.ncbi.nlm.nih.gov/19041189/
- Sacerdote P, et al. The opioid system in the modulation of immune responses. Int J Neuroprotection Neuroregeneration. 2008; 1(1):27‐28. https://www.ncbi.nlm.nih.gov/books/NBK6402/
- Sharafaddinzadeh N, et al. The effect of low dose naltrexone on quality of life of patients with multiple sclerosis: a randomized placebo-controlled trial. Mult Scler Relat Disord. 2010;8(4):305‐9. https://pubmed.ncbi.nlm.nih.gov/20534644/
- Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014 Apr;33(4):451-9. doi: 10.1007/s10067-014-2517-2. Epub 2014 Feb 15. PMID: 24526250; PMCID: PMC3962576. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3962576/
- Toljan K, Vrooman B. Low-Dose Naltrexone (LDN)-Review of Therapeutic Utilization. Med Sci (Basel). 2018 Sep 21;6(4):82. doi: 10.3390/medsci6040082. PMID: 30248938; PMCID: PMC6313374.https://pubmed.ncbi.nlm.nih.gov/30248938/
- Parker CE, Nguyen TM, Segal D, MacDonald JK, Chande N. Low dose naltrexone for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2018 Apr 1;4(4):CD010410. doi: 10.1002/14651858.CD010410.pub3. PMID: 29607497; PMCID: PMC6494424. https://pubmed.ncbi.nlm.nih.gov/29607497/
- Raknes G, Småbrekke L. Low dose naltrexone: Effects on medication in rheumatoid and seropositive arthritis. A nationwide register-based controlled quasi-experimental before-after study. PLoS One. 2019 Feb 14;14(2):e0212460. doi: 10.1371/journal.pone.0212460. Erratum in: PLoS One. 2019 Oct 1;14(10):e0223545. PMID: 30763385; PMCID: PMC6375629.https://pubmed.ncbi.nlm.nih.gov/30763385/
- Vuong C, Van Uum SH, O’Dell LE, Lutfy K, Friedman TC. The effects of opioids and opioid analogs on animal and human endocrine systems. Endocr Rev. 2010 Feb;31(1):98-132. doi: 10.1210/er.2009-0009. Epub 2009 Nov 10. PMID: 19903933; PMCID: PMC2852206. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2852206/
- Raknes G, Småbrekke L. No change in the consumption of thyroid hormones after starting low dose naltrexone (LDN): a quasi-experimental before-after study. BMC Endocr Disord. 2020 Oct 1;20(1):151. doi: 10.1186/s12902-020-00630-4. PMID: 33004044; PMCID: PMC7528597. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7528597/
