Unlocking the Secrets of Losing Weight with Adrenal Fatigue: A Comprehensive Guide
Ever felt like shedding belly fat is harder than rocket science? What if I told you there’s an undercover agent called ‘adrenal fatigue’ potentially sabotaging your efforts? Intrigued? You should be.
This is your all-access pass to cracking the code of losing weight with adrenal fatigue. We’ll be spilling the secrets nobody talks about. Buckle up, because it’s going to be a wild ride.
In this article, we’ll tackle these burning questions:
- What is adrenal fatigue and how does it affect your body?
- What’s the connection between adrenal fatigue and unexpected weight gain?
- Why is belly fat with adrenal fatigue more challenging than a Monday morning without coffee?
- How does cortisol, the ‘stress hormone,’ influence your weight?
- What role does blood sugar play in your weight management and adrenal issues?
- What are some proven strategies for losing weight with adrenal fatigue?
- “What’s really driving ‘adrenal fatigue’ and weight gain at a cellular level?”
And, of course, “What’s really driving ‘adrenal fatigue’ and weight gain at a cellular level?”
(Hint: we’re going to talk about mitochondria a lot)
Ready to unlock these secrets? Let’s dive in!
Understanding Adrenal Fatigue
Adrenal fatigue. Although many may argue it’s fiction, it’s a reality for many.
It may be more accurate to describe this as “cortisol issues” or even “HPA axis dysfunction,” but we’ll just say “adrenal fatigue” because that’s what most people resonate with.
What is Adrenal Fatigue?
Also known as adrenal exhaustion, adrenal fatigue is a health issue where the adrenal function is not up to par and results in a hormonal imbalance.
Now, again, adrenal fatigue doesn’t exist according to the conventional perspective (Cadegiani & Kater, 2016). But, we need a label for this collection of issues for the time being.
Either way, the symptoms are real. The question is what’s really going on…which we’ll get into later. So even if you have normal cortisol levels, pay attention!
For now, it’s important to know that people will feel tired, overwhelmed, and can’t keep up with their ‘go-go-go’ lifestyle.
Symptoms range from chronic fatigue and morning lethargy, digestive issues, to a strange craving for salty snacks.
Adrenal fatigue may lead to symptoms such as body aches, unexplained weight fluctuations, lower blood pressure, and even loss of body hair (Cadegiani & Kater, 2020).
So, if those symptoms resonate with you, then stick with us!
And, as we’ll discuss below, it’s not really an “adrenal” problem per se…

Role of Adrenal Glands
Now, what are these adrenal glands?
Picture them as tiny, yet mighty organs perched atop your kidneys. They’re in charge of producing crucial hormones, like cortisol (our stress hormone), and aldosterone, which helps manage blood pressure (Bornstein et al., 2016).
In essence, they’re unsung heroes keeping your body in equilibrium with all the stressors of life.
When they’re not working properly, things can go wonky in the body and can even result in tumors, autoimmune disorders, and medication-induced issues.
Don’t worry though, there’s light at the end of this tunnel!
We’re going to delve into how you can regain control over your body, beginning with understanding how adrenal fatigue is affecting your weight.
Adrenal Glands and Adrenal Fatigue Weight Gain
So, you’ve been trying to shed those extra pounds, but the scale seems stubborn or maybe you’re finding it’s way too easy to gain weight…either way, let’s talk about the possible culprit: your adrenals.
When You Can’t Lose Weight with Adrenal Fatigue: The Unseen Connection
When your adrenal glands are overworked, they produce more cortisol (the stress hormone). This can lead to increased appetite and decreased fat burning, and voila, it is hard to lose weight (Bose et al., 2009).
Stress, Cortisol, and Your Weight
There’s an unholy trinity of stress, adrenal fatigue, and weight gain.
Stress isn’t just a mental or emotional issue. It’s physical too.
When you’re stressed, your body goes into ‘fight or flight’ mode (remember the saber-toothed tiger chasing our ancestors?).
Eventually, this constant stress can lead to adrenal fatigue.
In this state, cortisol production spikes (before taking a nosedive), leading to an increased appetite.
Now, this appetite is typically for carbohydrates…

Why is that?
Your body will try to do whatever it can to survive on a short-term basis.
When your mitochondria are flopping, then fat burning is less efficient, but your body still needs to supply energy to function.
Thus, the only option remaining is to increase carbohydrate metabolism which starts with increasing your cravings for carbohydrate intake (Tomiyama et al., 2010).
And, what about the salt cravings?
That’s also related to your mitochondria!
The more water you have in your blood vessels from salt intake will lead to more water in your cells.
Hydrated cells are much more efficient cells at producing energy.
So, once again, a symptom (salt cravings) is tied to an energy production issue in your mitochondria.
Adrenal Fatigue and Your Metabolism
Think of your adrenal glands as the engine of your metabolism. When they’re overworked (hello, feeling stressed), your metabolic rate can drop.
This is a direct consequence of stress hormones overworking your mitochondria and they “shut down.”
This means fewer calories burned and more stored as fat. It’s like your body is preparing for a famine that isn’t coming (Kang et al., 2019).
With adrenal problems playing a starring role in your weight loss journey, let’s dial in the details on some key issues.
Lose Weight with Adrenal Fatigue: The Challenges
With adrenal fatigue, losing belly fat can feel like trying to climb Everest in flip-flops.
Why?
Two words: hormonal imbalance.
When your adrenals are overworked, they can go haywire, causing a domino effect on other hormone levels, including those regulating appetite and metabolism (Ranabir & Reetu, 2011).

Hormonal Imbalance and Weight Loss Resistance
It’s like this – issues with the adrenals can lead to high cortisol, which in turn can increase your appetite (Chao et al., 2011). It’s like your body is constantly whispering in your ear, “Hey, let’s eat!”
Also, imbalances in hormones like leptin and insulin can make it harder for your body to shed pounds (Rosenbaum & Leibel, 2014).
Fat cells make and release leptin. When your leptin receptors do not function properly, that’s when weight gain becomes the norm, and weight loss becomes a marathon without a finish line.
Here’s how things fall apart:
- Cortisol spikes too high
- This makes your body more resistant to leptin and insulin
- Appetite goes up and fat burning goes down
- You eat more
- This spikes cortisol more… and the downward cycle continues
Hence, you need to consider how to help re-balance these hormones.
Other Factors: Sleep, Diet, and Activity Levels
Beyond the hormones we mentioned there are other factors that play a part in your weight loss saga.
Cortisol issues often lead to sleep issues that further mess up your hunger hormones and make it hard to lose weight (Spiegel et al., 2004).
Not to mention when you’re feeling exhausted and just trying to get through your day, eating habits and physical activity can go by the wayside.
In other words, you’re human…. And not perfect.
More stress leads to more comfort seeking often through food and not getting enough physical activity (and you’re already exhausted).
So yes, losing the extra pounds with adrenal fatigue might be tougher than understanding the plot of Inception, but it’s not impossible…
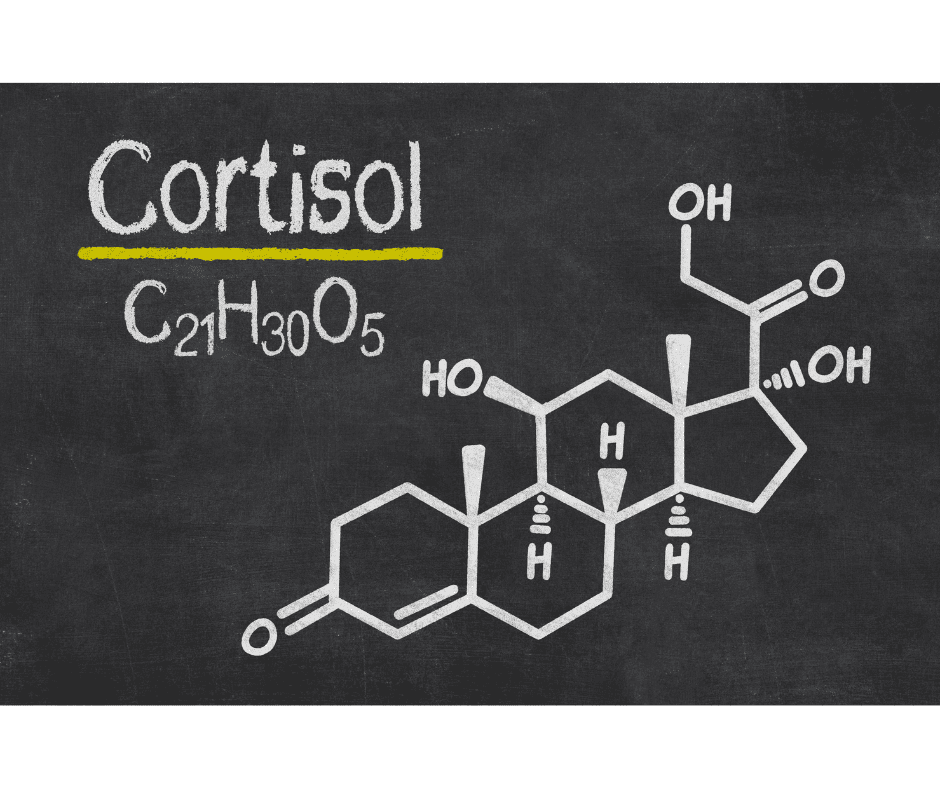
Cortisol: The Stress Hormone and Weight Management
Cortisol. It’s not just a buzzword thrown around in health circles. This little hormone plays a big role in your body, particularly when it comes to weight management and other health issues.
Cortisol: The Conductor of Your Body’s Orchestra
Picture cortisol as the conductor of your body’s orchestra. It keeps things in tune, managing how your body responds to stress and playing a crucial role in various bodily functions, like inflammation control and blood glucose regulation (Ranabir & Reetu, 2011).
Cortisol is a very important hormone that signals a cascade of important effects that are critical in the body.
Just ask someone with Addison’s Disease (primary adrenal insufficiency) where the importance of how cortisol works becomes very clear with dangerously low blood pressure, weakness, low blood sugar, electrolyte abnormalities, and more.

Needless to say, cortisol is a necessity to be able to regulate vital functions for life.
(Think of cortisol as a “survival” hormone)
The problem comes in when the adrenal glands aren’t making adjustments to day-to-day changes or even are stuck in one gear (high or low production) long term.
Cortisol Levels: A Balancing Act
Cortisol is like Goldilocks – it likes things ‘just right’.
Too little or too much can knock your body off balance.
As we’ve mentioned, high cortisol leads to increased appetite and altered metabolism, making your body more likely to store fat, especially around the abdomen (Epel et al., 2000).
(If you’ve ever taken prednisone or steroids long-term, you know that weight gain, especially belly fat, is one of the many unfortunate side effects.)
Chronically low cortisol can also do the same thing!
So, it’s imperative that you get your cortisol “just right.”
And the first step in doing that is…
Chronic Stress, Cortisol, and Weight Gain: The Unholy Trinity
It’s essential to have a discussion on stress when discussing cortisol.
Chronic stress can lead to high cortisol, creating a cycle that’s about as helpful for weight loss as a chocolate fountain at a diet convention. Over time, this can result in weight gain and difficulty shedding pounds (Björntorp, 2001).
So, managing the stress response and keeping cortisol in check isn’t just about feeling better – it’s a vital part of your adrenal fatigue weight loss journey.
And you may be thinking “yea, I already know I need to handle my stress…”
But, not everyone takes this as seriously as some of the flashy health items like supplements…
You must have solid strategies that can help to reduce the stress response such as:
- Breathing techniques
- Having an exercise routine
- Supporting the body with nutritious meals
- Or even breaking a vicious cycle of daily stressors that compound over time.

We’ll touch on this a bit more at the end… but if you don’t take stress management seriously, then you’ll be chasing other superficial “solutions.”
Blood Sugar and its Role in Weight Management and the Adrenals
It’s not just about calories. Managing your weight is also about keeping your blood sugar levels steady.
Here’s why: when your glucose levels spike, your body produces insulin to bring them down.
Over time, this can lead to insulin resistance, which can cause your body to store more fat and make weight loss harder (Polonsky, 1988).
That said, you don’t need to be hooked up to a glucose drip all day, follow a super restrictive diet, have continuous blood glucose monitoring, or even eat every hour to keep your blood glucose “steady.”
That is, worry less about the glucose you’re ingesting and more about the glucose your body is regulating.
(This is not an excuse to eat a bunch of sugar though…)
Blood Sugar and the Adrenals: A Complex Dance
Your adrenals are part of this complex dance.
They play a role in regulating your blood glucose levels, and constant spikes can put more stress on them. It’s like asking them to do a marathon every day (Marik & Bellomo, 2013).
So it is no surprise that certain foods such as junk food do not help insulin levels, energy levels, or the extra weight.
And, to make matters worse, when your cortisol levels swing when your adrenal axis is “off” then you’ll also have swings in blood sugar.

Maintaining Stable Blood Sugar: A Strategy for Adrenal Health and Weight Loss
So, how can we keep our sugar levels steady to support the adrenal function and weight loss?
Eating regular meals, choosing foods with a low glycemic index, and low-intensity regular exercise following eating are all good strategies (American Diabetes Association, 2020).
In other words, balance is key.
Just like you wouldn’t want to watch a movie with only action scenes or only romantic scenes, your body doesn’t want a diet of only highs or lows. It craves balance.
Now, what does “balance” mean for you? That’s a big question but an important one so stay tuned…
Strategies for Losing Weight (and how to stop gaining weight) with Adrenal Fatigue
Alright, let’s get to the good stuff. You’ve waded through the science, and now you’re ready for some action. Let’s talk about how to lose weight while trying to combat adrenal fatigue.
Surprise, lifestyle choices make an impact!
Now, this can be daunting for people who don’t want to change their habits. However, for those of you who are excited to know that there are things you can do, keep on reading.

Adrenal Fatigue Diet Tips: It’s Not Just About the Kale
First things first, diet. And no, we’re not talking about subsisting solely on kale and quinoa.
It’s all about balance with healthy foods: think lean proteins, complex carbs, and healthy fats.
I’m a bit biased, but a “paleo” style template is not a bad idea… just don’t forget the carbs.
(Seriously, going keto is an awful idea here)
Regular meals every 4 hours or so help maintain stable blood sugar levels, which is crucial for the adrenals (Hagobian & Braun, 2010).
Exercise and Stress Management: The Dynamic Duo
Next up, exercise and stress management. Think of them as Batman and Robin for your adrenals.
Regular physical activity can help manage cortisol levels, burn calories, promote weight loss, and with other health problems (Hill et al., 2003).
However, you want to remember this phrase when exercising:
“Exercise to stimulate, not to annihilate”

That is, you’ll do just enough exercise which can be annoying because you’re eager to lose weight.
However, you need to allow your engines to come back online before throwing them into “turbo mode.”
If you don’t resist the urge to be “reasonable” with exercise, then you’ll perpetuate the cycle of stress and burning out.
Now, what should you do for stress management?
I would highly recommend taking what works for you.
Many of our clients will find one that works the best for them whether that is yoga, breathwork, etc.
So, the actual practice itself is not important by itself.
You need to find what works for you and then be consistent!

Seriously… every dang day and twice on the extra stressful days.
Now, you’d be wise to use these stress techniques when your cortisol is the most elevated to keep them in check (Pascoe et al., 2017).
Sleep: The Unsung Hero
Finally, let’s talk about sleep. It’s not just for beauty—it’s also vital for weight loss and adrenal health. Poor sleep can cause hormone imbalance, leading to weight gain, increased stress, and other health conditions (Spiegel et al., 2004).
Let’s be real, cortisol is a circadian hormone and the circadian rhythm plays an important role in the timing of when the body releases cortisol.
Low cortisol at night is important for restful sleep. Higher cortisol levels are necessary in the morning so that you’re not feeling like a spare tire.
So, make sure to use the above strategies to get your cortisol levels low for bedtime and, then, as a result, they should normalize more in the AM.
So, there you have it.
Simple, right? (Just kidding, we know it’s not. But hey, every journey starts with a single step!)

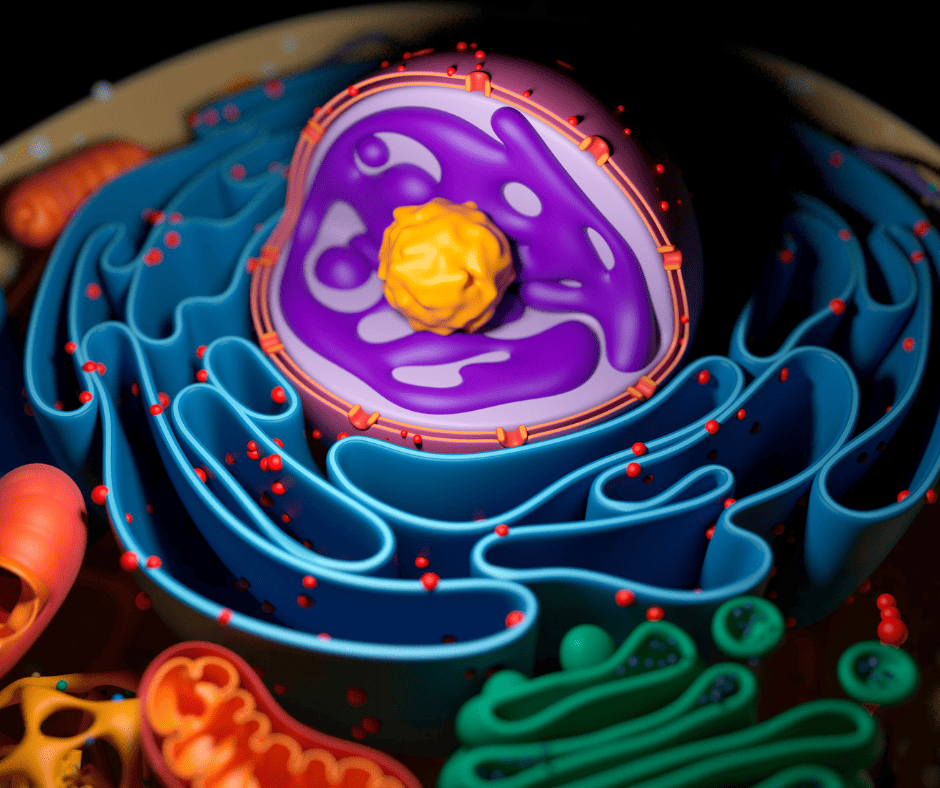
Mitochondria and Circadian Rhythms – Beyond the Basics
Now, everything we talked about above is all connected to the same core factor: your mitochondria.
When your mitochondria are producing enough energy, then that leads to an “emergency signal” to your body.
And, how does your body respond?
With cortisol and other stress hormones!
And, your body’s circadian rhythm is what naturally dictates when you should be secreting cortisol (and all the other hormones we talked about).
So, when your circadian rhythm is off, then your cortisol is off.
Here’s the rub…
You can do everything mentioned above, but if you’re not targeting your mitochondria and circadian rhythms, then you’ll have limited success in rebuilding your health.
That’s why we made a short training on your mitochondria and circadian rhythms here:
https://optimalcircadianhealth.com/learn/
Enjoy!

Written By: Dylan Petkus, MD, MPH, MS
Dr. Dylan Petkus is on a mission to help people overcome their health issues like sleep apnea so they are not limited by their condition or trapped by options that don’t provide full resolution.
He earned his Master’s of Science in Physiology at Pennsylvania State University where he was awarded a research fellowship and was a peer-reviewed published author. He went on to earn both his Master’s in Public Health and Medical Degree from the University of Miami Miller School of Medicine. Thereafter, he specialized in Family Medicine to help patients on the front-line of chronic disease.
Having overcome his own health challenges, including sleep apnea, he strives to help empower others to live fuller, healthier lives.
References:
Cadegiani, F. A., & Kater, C. E. (2016). Adrenal fatigue does not exist: a systematic review. BMC Endocrine Disorders, 16(1), 48. https://doi.org/10.1186/s12902-016-0128-4
Bornstein, S. R., Allolio, B., Arlt, W., et al. (2016). Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology & Metabolism, 101(2), 364-389. https://doi.org/10.1210/jc.2015-1710
Cadegiani, F. A., & Kater, C. E. (2020). Basal Hormones and Biochemical Markers as Predictors of Overtraining Syndrome in Male Athletes: The EROS-BASAL Study. Journal of Athletic Training, 55(9), 930-939.https://pubmed.ncbi.nlm.nih.gov/31386577/
Bose, M., Olivan, B., & Laferrere, B. (2009). Stress and obesity: the role of the hypothalamic-pituitary-adrenal axis in metabolic disease. Current Opinion in Endocrinology, Diabetes and Obesity, 16(5), 340-346. https://doi.org/10.1097/MED.0b013e32832fa137
Tomiyama, A. J., Dallman, M. F., & Epel, E. S. (2010). Comfort food is comforting to those most stressed: evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology, 36(10), 1513-1519.https://pubmed.ncbi.nlm.nih.gov/21906885/
Kang, S., Lee, S. P., & Kim, S. J. (2019). Chronic intermittent hypoxia induces liver fibrosis in mice with diet-induced obesity via TLR4/MyD88/MAPK/NF-kB signaling pathways. Biochemical and Biophysical Research Communications, 514(1), 53-59.https://pubmed.ncbi.nlm.nih.gov/28623125/
Ranabir, S., & Reetu, K. (2011). Stress and hormones. Indian Journal of Endocrinology and Metabolism, 15(1), 18. https://doi.org/10.4103/2230-8210.77573
Chao, A. M., Jastreboff, A. M., White, M. A., Grilo, C. M., & Sinha, R. (2017). Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight. Obesity, 25(4), 713-720. https://doi.org/10.1002/oby.21790
Rosenbaum, M., & Leibel, R. L. (2014). 20 years of leptin: role of leptin in energy homeostasis in humans. Journal of Endocrinology, 223(1), T83-T96. https://doi.org/10.1530/JOE-14-0358
Spiegel, K., Tasali, E., Penev, P., & Van Cauter, E. (2004). Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine, 141(11), 846-850. https://doi.org/10.7326/0003-4819-141-11-200412070-00008
Donnelly, J. E., Blair, S. N., Jakicic, J. M., Manore, M. M., Rankin, J. W., & Smith, B. K. (2009). Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine and Science https://sci-hub.st/10.1249/MSS.0b013e3181949333
Epel, E., Lapidus, R., McEwen, B., & Brownell, K. (2001). Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology, 26(1), 37-49. Link
Björntorp, P. (2001). Do stress reactions cause abdominal obesity and comorbidities? Obesity Reviews, 2(2), 73-86. Link
Polonsky, K. S. (1988). The dynamics of insulin secretion in obesity and diabetes. International Journal of Obesity, 12(2), 111-122. Link
Marik, P. E., & Bellomo, R. (2013). Stress hyperglycemia: An essential survival response!. Critical Care, 17(2), 305. Link
American Diabetes Association. (2020). 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care, 43(Supplement 1), S14-S31. Link
Hagobian, T. A., & Braun, B. (2010). Physical activity and hormonal regulation of appetite: sex differences and weight control. Exercise and Sport Sciences Reviews, 38(1), 25-30. Link
Hill, J. O., Wyatt, H. R., & Peters, J. C. (2013). Energy balance and obesity. Circulation, 126(1), 126-132. Link
Pascoe, M. C., Thompson, D. R., & Ski, C. F. (2017). Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology, 86, 152-168. Link