Sleep Tight: Uncovering the Top Supplements for Sleep Apnea
You’re trying to get a good night’s rest, but your body has other plans.
Frustrating, right?
But fear not, we’re here to help.
In this article, we’ll dive into this sleep disorder and how supplements might just be the secret weapon you’ve been missing.
So, buckle up (or should we say, tuck in?) as we answer the big questions:
- What’s the deal with sleep and why is sleep apnea a party pooper?
- Can vitamins and minerals really make a difference in sleep health?
- What are the top supplements for sleep apnea, and what’s the scoop behind them?
- How does sleep apnea tango with your immune function, and can supplements cut in?
- What’s the link between sleep apnea, brain health, and supplements?
- How can you safely integrate supplements into your sleep apnea management plan?
If you’re tired of counting sheep and ready for some real Z’s, read on!
Understanding Sleep and Sleep Apnea
Sleep, it’s like the oil in your body’s engine. Without it, everything starts to grind and stutter (Chattu, Manzar, Kumary, Burman, Spence, & Pandi-Perumal, 2018). It’s not just about feeling refreshed – quality sleep is key to our cognitive function, emotional well-being, and overall health (Medic, Wille, & Hemels, 2017).
Enter sleep apnea, the notorious thief of peaceful nights. It’s a condition where your breathing stops and starts repeatedly as you slumber. Think of it as a mischievous elf that blocks your airways every now and then (Benjafield et al., 2019).
But it’s not just about noisy snoring or feeling groggy the next day. Is linked with a host of not-so-fun health conditions. It’s like that one guy who never shows up to the party, bringing along his friends: heart disease, hypertension, diabetes, and depression (Lévy, Kohler, McNicholas, Barbé, McEvoy, & Somers, 2015).
And with this, we’ve just scratched the surface. Stick around as we dive deeper into this nighttime nuisance and the potential of supplements to help manage it.
Decoding Sleep Apnea
Picture sleep apnea as the invisible gremlin playing a discordant tune on your body’s orchestra. It’s a disorder punctuated by sudden halts and resumptions in breathing during sleep (Senaratna et al., 2017).
Symptoms? They can be sly – boisterous snoring, daytime fatigue, and awakening with a gasping or choking sensation. It’s easy to brush it off as just being a lousy sleeper. Sorry to burst the bubble, but it’s our little gremlin friend stirring up trouble (Peppard et al., 2013).

Wondering about the prevalence of this unwelcome guest? It’s more widespread than you’d expect. Nearly 1 billion people worldwide aged 30-69 years are estimated to have obstructive sleep apnea (Benjafield et al., 2019). What increases the risk? Factors include obesity, smoking, alcohol use, and even the genes passed down from your ancestors (Peppard et al., 2013).
Eager to show sleep apnea the exit? Stay tuned as we dig deeper into the details and explore how supplements may help you reclaim your night
The Importance of Sleep Quality
Let’s talk about sleep quality. It’s not just about getting your eight hours in; it’s about how well you snooze when the lights go out. Quality sleep is like a power-up for your body – it improves cognition, bolsters your immune system, and even helps keep your heart healthy (Irwin, 2019).
Now, let’s connect the dots with sleep apnea. Picture this: you’re in a peaceful slumber, dreaming about winning the lottery, when suddenly, you’re gasping for air. Not exactly a recipe for a good night’s sleep, is it?
This can severely disrupt REM sleep, which is a crucial phase of the sleep cycle, during which dreams occur and the brain processes memories (Rosenzweig et al., 2016).

During REM sleep sleep apnea episodes often intensify, leading to a severe drop in oxygen levels (Javaheri, 2017). This occurs due to the loss of muscle tone that characterizes this sleep stage. This can cause the airways to narrow or collapse more easily, exacerbating apnea symptoms (Joosten et al., 2014).
Needless to say, turns your restful night into an obstacle course, leading to poor sleep quality and leaving you feeling more like a zombie than a refreshed, ready-to-take-on-the-day human being (Kendzerska et al., 2014), but I’m sure we don’t need to tell you that.
So, remember, quality sleep isn’t just a luxury—it’s a necessity. Your body will thank you for it!
Sleep Disordered Breathing (SDB): A Closer Look
It’s like a troublesome cousin to sleep apnea – they’re related, but with some key differences. SDB encompasses a range of breathing issues during sleep, of which sleep apnea is a notorious member (Senaratna et al., 2017).
It’s not just about the loud snoring (although, let’s be honest, that’s pretty disruptive too!). SDB can lead to low oxygen levels, fragmented sleep, and all-around bad vibes for your health. No surprise, when your body is unable to recover properly at night, whether that’s the brain function, heart, muscles, and more, you end up with cognitive impairments, high blood pressure, blood sugar abnormalities, and cardiovascular disease (Peppard et al., 2013).
Now, in case you want to start addressing this now, we’ve developed breathing exercises that promote easy nighttime breathing and put all of those resources for you in the Sleep Apnea Solution Book. The breathing routines have written instructions you can follow step-by-step or you can just press play and follow along the audio track to walk you through nighttime breathing exercises. Make it easy to boost natural breathing at night and take the first steps towards better sleep.
Delving Deeper: Obstructive Sleep Apnea (OSA)
OSA is the most common form of sleep apnea, where your throat muscles intermittently relax, blocking your airway (Senaratna et al., 2017). Faster breathing makes this more likely to happen by pulling the tongue into the airway like a suction effect, blocking off the airway like you can see below.

But don’t lose sleep over it (pun intended!). Understanding the problem is half the battle won. The other half? Well, that’s what the rest of this article is for!
Sleep Apnea Doesn’t Discriminate
While it’s a common belief that sleep apnea is a byproduct of being overweight because studies have shown that people with neck thickness and higher BMI have a greater risk (Peppard et al., 2000), it’s crucial to remember that sleep apnea is an equal opportunity annoyer. It doesn’t discriminate, folks! People of all ages, sizes, and neck circumferences can have sleep apnea (Lurie, 2011).
You may be surprised to know that even lean individuals and children can suffer from this condition (Kapur et al., 2002). So, remember, this is not just a ‘big guy’ problem. It’s a ‘big problem’ for guys (and gals) of all sizes!
A curious thought, isn’t it? It’s not just about a deviated septum, thick neck, or large waistline (Caples et al., 2005). Now, brace yourself for a real mind-bender.
What’s Really Going on with Sleep Apnea
What if sleep apnea is actually a compensatory mechanism, a sort of a body’s DIY defense plan against further damage? Here’s the curveball – what if the body, in its wisdom, is trying to protect itself from the harm of… oxygen?
Yep, oxygen, that life-giving stuff, can sometimes play the villain (Droge, 2002). In states of high inflammation, oxygen can morph into free radicals, causing damage (Kohen & Nyska, 2002). Imagine sleep apnea as the body’s attempt to shield its precious mitochondria (those little cellular powerhouses that use oxygen) from this harm.
Remember, the mitochondria produce melatonin and produce energy (also known as adenosine triphosphate or ATP). Energy is critical for endless functions in the body including but not limited to immune health and restful sleep.
Now, if this were true, our current strategies for researching sleep apnea are misguided and more research is needed.
That would also mean our current approach to treatment, which is about getting more oxygen into the body, could be somewhat misguided as well.
So, this is where it makes sense to consider additional options, like supplements, to address the underlying reasons for the body’s compensatory mechanisms (Kheirandish-Gozal & Gozal, 2014).
Remember though, supplements are just the tip of the iceberg in what’s needed to address this issue. But hey, they’re worth mentioning, so let’s dive in, shall we?
Vitamins: Addressing the “Root Cause”
Now, let’s talk about vitamins. Imagine vitamins as a pack of multi-talented superheroes, each with a unique power, all dedicated to the mission of health. A number of these superheroes play a crucial role in sleep health (Grandner et al., 2010).
So, could pumping up your vitamin intake help poor sleep quality?
Perhaps, in continuing this conversation we want to keep in mind, the following questions:
- Why are these vitamins low in the first place?
- Are replacing these vitamins going to solve the underlying issue?
- Are taking these vitamins supplement going to have the intended effect?
Let’s explore further!
Top Nutritional Supplements for Sleep Apnea
Alright, it’s time for the main event: the top nutritional supplements for sleep apnea.
Magnesium

First up, we have magnesium supplements, the body’s natural chill pill. This essential mineral is involved in over 300 enzymatic reactions in the body, including those that regulate sleep. Studies have shown that magnesium can help improve sleep efficiency and sleep time, especially in those with insomnia; on the flip side, a magnesium deficiency can result in insomnia and SDB, so topping up might just help out (Abbasi et al., 2012).
Adequate intake of magnesium is fun because there are so many factors that influence it being depleted and many different types that can be supplemented.
Types and Typical Dosages:
- Magnesium Citrate: Commonly used to support digestive health. Typical dosage: 200-400 mg per day.
- Magnesium Glycinate: Known for its calming effects and higher bioavailability. Typical dosage: 200-400 mg per day.
- Magnesium Oxide: Often used as a laxative or for heartburn relief. Typical dosage: 250-500 mg per day.
- Magnesium Threonate: Noted for its potential cognitive benefits. Typical dosage: 1,000-2,000 mg per day.
- Magnesium Malate: Sometimes used for muscle pain and fatigue. Typical dosage: 1,200-2,400 mg per day.
In what foods can you find this sleep-supporting superstar? Well, it’s present in a variety of foods. If you’re looking for vegetables, leafy greens like spinach and chard are a great source. You’ll also find magnesium in nuts and seeds, particularly pumpkin seeds. Whole grains and legumes, with black beans and quinoa being particularly high in magnesium. Even dark chocolate can give you a magnesium boost, in case you need another excuse to have a square or two (or three)!
Vitamin D
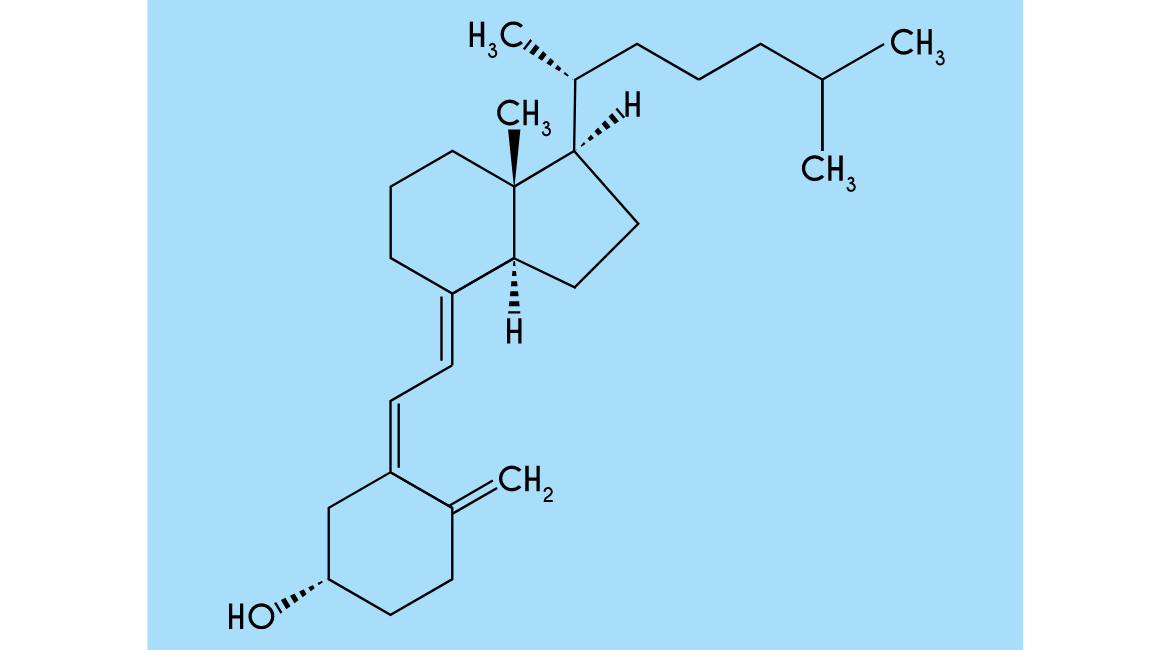
Next, we have vitamin D, which is actually a hormone! While vitamin D’s role in bone health, mood regulation, and how it supports immune health is best known, recent research has also suggested a link between vitamin D deficiencies and sleep disorders, including sleep apnea (McCarty et al., 2012).
One study found a significant correlation between low serum vitamin D levels and the severity of obstructive sleep apnea. The study suggested that vitamin D deficiency could contribute to the pathogenesis of sleep apnea, possibly by promoting inflammation and affecting the muscles that control our airways (Kerley et al., 2020). However, the connection isn’t entirely clear-cut, and more research is needed.
Types and Typical Dosages:
- Vitamin D2 (Ergocalciferol): Plant-based form. Typical dosage: 400-2,000 IU per day.
- Vitamin D3 (Cholecalciferol): Animal-based form, considered more effective. Typical dosage: 1,000-4,000 IU per day.
What I can tell you from my experience is that inflammation is sky high in people with sleep apnea. Vitamin D is a potent anti-inflammatory. However, I don’t love vitamin D in a supplement form. I much prefer natural sources such as the sun and some food sources of vitamin D such as fish skin, fish eye, egg yolks, and mushrooms.
Fish Oils

Let’s not forget omega-3 fatty acids. Yes, the stuff in fish oil. A study found that children with high blood levels of omega-3s had fewer sleep disturbances and a lower risk of sleep apnea (Montgomery et al., 2014). Omega-3 are prevalent and also known as fish oil supplements. Dietary sources of these beneficial fatty acids can, surprise, be obtained from fatty fish.
Types and Typical Dosages:
- Eicosapentaenoic Acid (EPA): Typically found in fish oil. Typical dosage: 250-500 mg per day.
- Docosahexaenoic Acid (DHA): Also found in fish oil. Typical dosage: 250-500 mg per day.
- Alpha-linolenic Acid (ALA): Plant-based omega-3, found in flaxseeds, chia seeds, and walnuts. Typical dosage: 1,000-2,000 mg per day.
Tryptophan
Then there’s tryptophan, an amino acid that the body converts into the sleep hormone melatonin. Research suggests that tryptophan supplements can improve sleep and may be beneficial for sleep apnea (Hartmann, 1982). Tryptophan can be taken as a supplement, or it can be found in foods like turkey. There’s nothing like a nice post-Thanksgiving nap!
Types and Typical Dosages:
- L-Tryptophan: Commonly used form. Typical dosage: 500-1,000 mg per day.
Vitamin C

In the red corner, we have vitamin C, also known as ascorbic acid. It is perhaps most well known for how it supports immune health. Vitamin C is a stalwart champion in the health world and has been implicated in a study showing that it can mitigate some of the oxidative stress caused by sleep apnea (Lavie et al., 2009).
Types and Typical Dosages:
- Ascorbic Acid: Most common form. Typical dosage: 500-1,000 mg per day.
- Sodium Ascorbate: Buffered form, less acidic. Typical dosage: 1,000-2,000 mg per day.
- Calcium Ascorbate: Buffered form with added calcium. Typical dosage: 1,000-2,000 mg per day.
Don’t forget about the many food sources for vitamin C that include citrus fruits, bell peppers, strawberries, and broccoli. Who knew having healthy sleep could be so tasty? Now don’t forget herbal tea for sleep apnea. Some can contain vitamin C and have other benefits as well.
Vitamin E

In the blue corner, we have vitamin E. This is another powerful antioxidant that plays a crucial role in protecting the body’s cells from damage. Research suggests that vitamin E, along with vitamin C, may reduce blood pressure in patients with sleep apnea (Tan et al., 2013).
Types and Typical Dosages:
- Alpha-Tocopherol: Most common form. Typical dosage: 15-400 IU per day.
- Mixed Tocopherols: Includes alpha, beta, gamma, and delta forms. Typical dosage: 400-800 IU per day.
- Tocotrienols: Less common form with potentially higher antioxidant properties. Typical dosage: 50-200 mg per day.
But be careful! Antioxidant supplements like vitamin C and vitamin E can be double-edged swords. While vitamin E is an antioxidant and important for many body functions, it’s a bit like that friend who always insists on picking the karaoke song – great in the right doses but can cause some trouble if overdone. Think of free radicals as a bit like fire in a fireplace. When the fire is contained, it’s helpful and warming. When it’s out of control, it’s destructive. In a similar way, free radicals, while essential for cellular function and communication, can cause havoc when in excess (Lobo et al., 2010).
While vitamin E does combat free radicals, high doses of vitamin E supplementation have been associated with certain health risks, such as hemorrhagic stroke and even increased mortality (Bjelakovic et al., 2014). Vitamin E has also been linked to an increased risk of certain types of cancer, particularly prostate cancer in men (Klein et al., 2011). It’s like trying to put out a forest fire with a garden hose – it’s not addressing the root of the problem. Instead, we should aim to curb the uncontrolled production of free radicals, often due to high inflammation.
Remember, it’s not just about putting out the fire, it’s about preventing the spark in the first place. Remember this principle for vitamin E, vitamin C, and other antioxidants as well! Now that you know about some of the risks in supplementing vitamin E, it is safer to say that it is harder to go wrong with sources, including foods like almonds, spinach, and sweet potatoes.
If you want to learn how to make breathing easier naturally, get the Sleep Apnea Solution Book. It covers the top nutrition, environmental, circadian, and nervous system keys for sleep apnea.
B Vitamins: Vitamin B1

First we’ll turn our attention to thiamine, also known as vitamin B1 (most commonly in the form of thiamine hydrochloride). Thiamine plays a crucial role in energy metabolism and the growth, development, and function of cells (Frank, 2019).
Types and Typical Dosages:
- Thiamine Hydrochloride: Commonly used form. Typical dosage: 1.1-1.2 mg per day.
- Thiamine Mononitrate: Another common form. Typical dosage: 1.1-1.2 mg per day.
- Benfotiamine: Fat-soluble form with higher bioavailability. Typical dosage: 150-300 mg per day.
But, is there a connection between thiamine supplementation and sleep apnea? While there’s no other research suggesting thiamine supplementation can alleviate symptoms, studies show thiamine deficiency can cause a range of neurological issues, some of which can indirectly affect sleep quality (Frank, 2019).
However, it’s crucial to remember that more research is needed to fully understand the potential impact of thiamine on sleep apnea.
B Vitamins: Vitamin B6
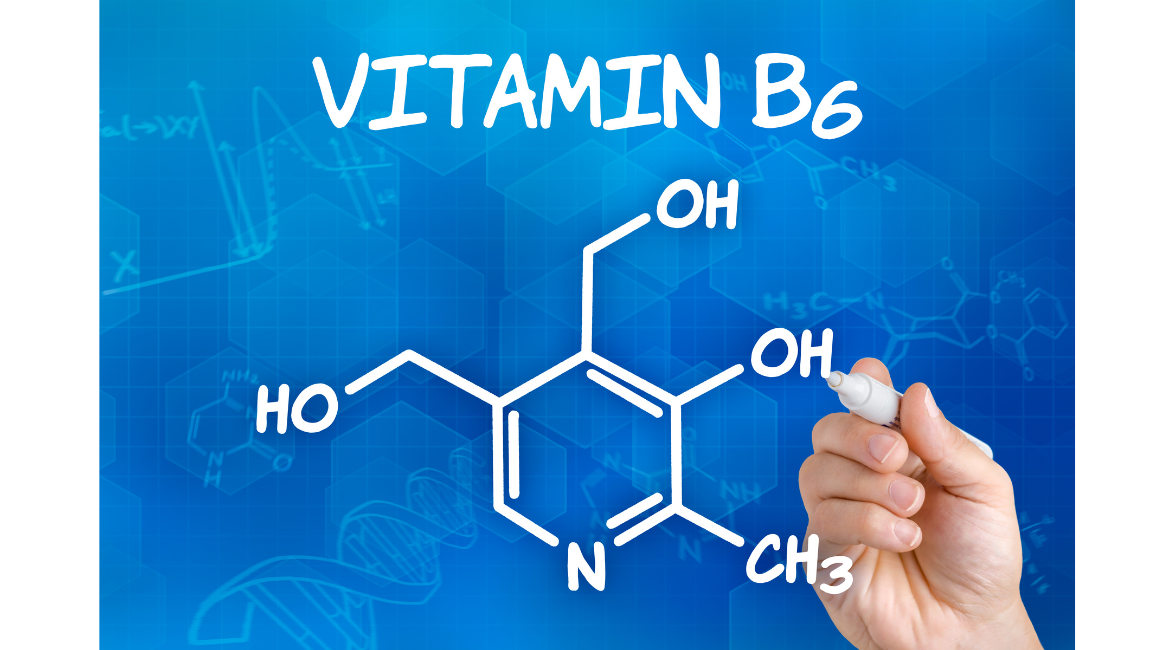
You see, vitamins like B6 and B12 have been noted to directly or indirectly influence sleep quality. Vitamin B6, for example, is an essential player in the production of serotonin, a hormone that moonlights as a sleep regulator (Birdsall, 1998).
Types and Typical Dosages:
- Pyridoxine Hydrochloride: Most common form. Typical dosage: 1.3-2.0 mg per day.
- Pyridoxal-5-Phosphate (P5P): Active form of vitamin B6. Typical dosage: 20-50 mg per day.
Dietary sources of vitamin B6 are similar to other b vitamins: chicken, turkey, beef, seafood, bananas, avocados, spinach, potatoes, legumes and whole grains.
B Vitamins: Vitamin B9

Next up on our list of b vitamins is folic acid, more commonly known as vitamin B9.
Folic acid is crucial for cell growth, metabolism, and the white and red blood cell formation in the bone marrow (Tamura & Picciano, 2006).
Types and Typical Dosages:
- Folic Acid: Synthetic form. Typical dosage: 400-800 mcg per day.
- 5-Methyltetrahydrofolate (5-MTHF): Active form of folate. Typical dosage: 400-800 mcg per day.
Now, theoretically more red blood cells would increase the oxygen carrying capacity in people apneic episodes, but more research is needed as many of the current studies focus on the broader B vitamins group, not specifically folic acid.
However, considering folic acid’s crucial role in overall health and wellbeing, it’s plausible that a deficiency could affect sleep patterns.
B Vitamins: Vitamin B12

Meanwhile, vitamin B12 has been linked to the regulation of the sleep hormone melatonin, your body’s natural Sandman (Okawa et al., 1997).
One study found that Vitamin B12 deficiency was more prevalent in patients with OSA (Gozal et al., 2013).
Types and Typical Dosages:
- Cyanocobalamin: Most common and stable form. Typical dosage: 2.4 mcg per day.
- Methylcobalamin: Active form, often used for neurological health. Typical dosage: 1,000-5,000 mcg per day.
- Adenosylcobalamin: Another active form, important for mitochondrial health. Typical dosage: 1,000-5,000 mcg per day.
It is Important to note that B vitamins are found in a healthy diet with a wide range of food sources, including whole grains, meat, egg yolks, legumes, seeds, and nuts. So a B complex vitamin is not the only option.
Melatonin
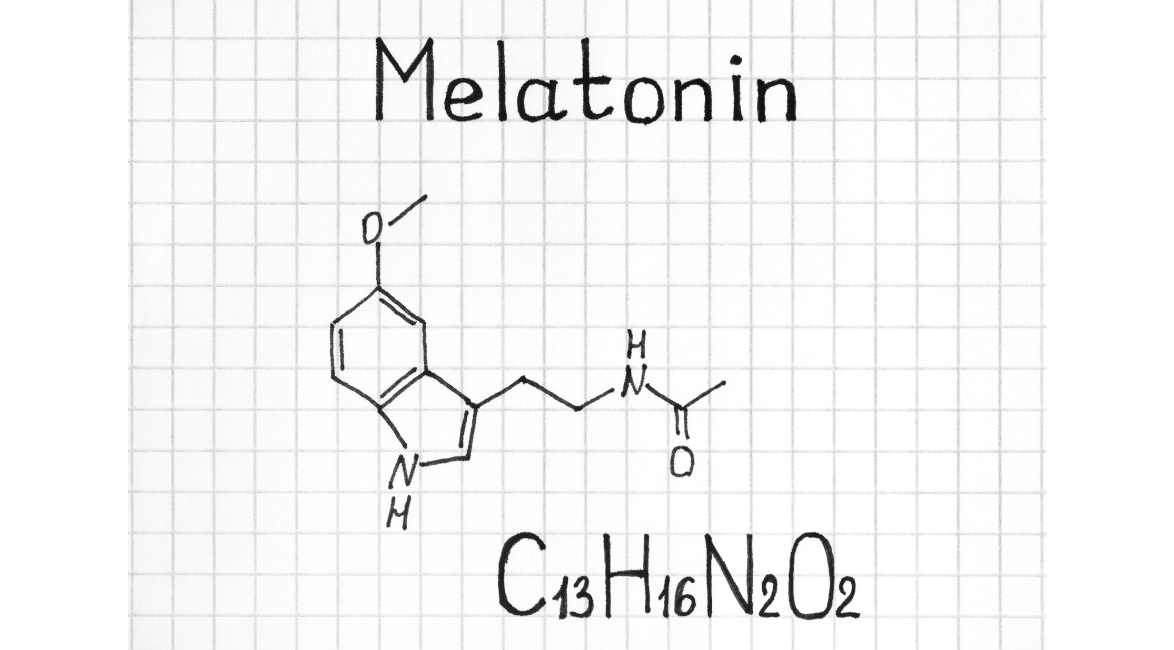
Ah, melatonin, the body’s in-house sandman, famous for its role in regulating our sleep-wake cycles and circadian rhythm.
Yet research is limited regarding sleep apnea and melatonin. A study evaluated the efficacy and safety of prolonged-release melatonin in insomnia patients aged 55 years and older and showed improved sleep quality and alertness, but did not specifically focus on sleep apnea (Lemoine et al., 2007).
Types and Typical Dosages:
- Immediate-Release Melatonin: Helps with falling asleep. Typical dosage: 0.5-5 mg per day.
- Prolonged-Release Melatonin: Helps with staying asleep. Typical dosage: 2-10 mg per day.
However, it’s crucial to remember that while supplemental melatonin may have short term benefits for some people, taking this hormone as a supplement does not come without consequences.
While melatonin is generally considered safe for short-term use, it’s not without its potential downsides (Andersen et al., 2016). Side effects can include headache, dizziness, nausea, and drowsiness. There’s also the possibility of melatonin interacting with various medications including anticoagulants, immunosuppressants, diabetes medications and birth control pills (Auld et al., 2017).
Long-term use is less well-studied, and there’s some concern that extended melatonin use might suppress the body’s own production of the hormone, impacting the circadian rhythm (Srinivasan et al., 2011). Because melatonin is so important for the circadian clock, we’d recommend proceeding cautiously with supplemental forms.
Another reason to proceed with caution is that melatonin can relax the muscles in your airways too much leading to collapse. So, tread lightly!
Sleep Supplement Important Note

Remember, while supplements like vitamins and essential minerals can be beneficial, getting these nutrients from a balanced diet is usually the best way to go. Food sources provide a complex matrix of vitamins, minerals, fiber, and other substances that work together to promote good health.
Now, remember, supplements aren’t a magic bullet. They’re one part of the puzzle. A healthy lifestyle, including good sleep hygiene, is also crucial in having healthy sleep.
And of course, as with any supplementation plan, it’s always wise to discuss with your healthcare professional before starting a supplement. They can help you determine the correct dosage and monitor your progress, ensuring you get the most benefit while minimizing any potential risks.
Conclusion
In conclusion, managing sleep apnea effectively often involves a multifaceted approach that includes dietary and lifestyle changes, along with considering various supplements. We’ve explored the potential benefits of key supplements like magnesium, vitamin D, fish oils, tryptophan, vitamin C, vitamin E, and B vitamins, all of which play significant roles in supporting better sleep and overall health. Each of these nutrients can address specific aspects of sleep apnea, from reducing inflammation to regulating sleep-wake cycles and enhancing oxygen delivery.
Encouragingly, supplements can be a valuable addition to your sleep apnea management strategy. By ensuring your body receives the right nutrients, you can support your health and possibly reduce the severity of sleep apnea symptoms. However, it’s essential to approach supplementation thoughtfully and consult with healthcare professionals when making changes to your regimen.
Ready to take control of your sleep health? Check out our comprehensive book, which not only delves deeper into the best supplements for sleep apnea but also includes the most effective breathing routines. With accompanying audio tracks, you can start implementing these techniques tonight and work towards achieving the restful sleep you deserve. Don’t wait—start your journey to better sleep now!

References:
- Chattu, V. K., Manzar, M. D., Kumary, S., Burman, D., Spence, D. W., & Pandi-Perumal, S. R. (2018). The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare, 7(1), 1. https://pubmed.ncbi.nlm.nih.gov/30577441/
- Medic, G., Wille, M., & Hemels, M. E. (2017). Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep, 9, 151–161. https://pubmed.ncbi.nlm.nih.gov/28579842/
- Benjafield, A. V., Ayas, N. T., Eastwood, P. R., Heinzer, R., Ip, M. S., Morrell, M. J., … & Pépin, J. L. (2019). Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet Respiratory Medicine, 7(8), 687-698. https://pubmed.ncbi.nlm.nih.gov/31300334/
- Lévy, P., Kohler, M., McNicholas, W. T., Barbé, F., McEvoy, R. D., & Somers, V. K. (2015). Obstructive sleep apnoea syndrome. Nature Reviews Disease Primers, 1(1), 1-19. https://pubmed.ncbi.nlm.nih.gov/27188535/
- Senaratna, C. V., Perret, J. L., Lodge, C. J., Lowe, A. J., Campbell, B. E., Matheson, M. C., … & Dharmage, S. C. (2017). Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Medicine Reviews, 34, 70-81. https://pubmed.ncbi.nlm.nih.gov/27568340/
- Peppard, P. E., Young, T., Barnet, J. H., Palta, M., Hagen, E. W., & Hla, K. M. (2013). Increased prevalence of sleep-disordered breathing in adults. American journal of epidemiology, 177(9), 1006-1014. https://pubmed.ncbi.nlm.nih.gov/23589584/
- Irwin, M. R. (2019). Why sleep is important for health: a psychoneuroimmunology perspective. Annual review of psychology, 66, 143-172. https://pubmed.ncbi.nlm.nih.gov/25061767/
- Rosenzweig, I., Glasser, M., Crum, W. R., Kempton, M. J., Milosevic, M., McMillan, A., … & Morrell, M. J. (2016). Changes in neurocognitive architecture in patients with obstructive sleep apnea treated with continuous positive airway pressure. EBioMedicine, 7, 221-229. https://pubmed.ncbi.nlm.nih.gov/27322475/
- Javaheri, S. (2017). Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. Journal of the American College of Cardiology, 69(7), 841-858. https://pubmed.ncbi.nlm.nih.gov/28209226/
- Joosten, S. A., O’Driscoll, D. M., Berger, P. J., & Hamilton, G. S. (2014). Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep medicine reviews, 18(1), 7-17. https://pubmed.ncbi.nlm.nih.gov/23669094/
- Kendzerska, T., Gershon, A. S., Hawker, G., Leung, R. S., & Tomlinson, G. (2014). Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med, 11(2), e1001599. https://pubmed.ncbi.nlm.nih.gov/24503600/
- Peppard, P. E., Young, T., Palta, M., & Skatrud, J. (2000). Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine, 342(19), 1378-1384. https://pubmed.ncbi.nlm.nih.gov/10805822/
- Young, T., Palta, M., Dempsey, J., Skatrud, J., Weber, S., & Badr, S. (1997). The occurrence of sleep-disordered breathing among middle-aged adults. New England Journal of Medicine, 336(17), 1230-1235. https://pubmed.ncbi.nlm.nih.gov/8464434/
- Kapur, V., Strohl, K. P., Redline, S., Iber, C., O’connor, G., & Nieto, J. (2002). Underdiagnosis of sleep apnea syndrome in US communities. Sleep and Breathing, 6(2), 49-54. https://pubmed.ncbi.nlm.nih.gov/12075479/
- Caples, S. M., Gami, A. S., & Somers, V. K. (2005). Obstructive sleep apnea. Annals of Internal Medicine, 142(3), 187-197. https://pubmed.ncbi.nlm.nih.gov/15684207/
- Dröge, W. (2002). Free radicals in the physiological control of cell function. Physiological Reviews, 82(1), 47-95. https://pubmed.ncbi.nlm.nih.gov/11773609/
- Kohen, R., & Nyska, A. (2002). Oxidation of biological systems: oxidative stress phenomena, antioxidants, redox reactions, and methods for their quantification. Toxicologic Pathology, 30(6), 620-650. https://pubmed.ncbi.nlm.nih.gov/12512863/
- Kheirandish-Gozal, L., & Gozal, D. (2014). Obstructive sleep apnea and inflammation: proof of concept based on two illustrative cytokines. International Journal of Molecular Sciences, 15(2), 2925-2938. https://pubmed.ncbi.nlm.nih.gov/30678164/
- Grandner, M. A., Jackson, N., Gerstner, J. R., & Knutson, K. L. (2014). Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite, 64, 71-80. https://pubmed.ncbi.nlm.nih.gov/23339991/
- Birdsall, T. C. (1998). 5-Hydroxytryptophan: a clinically-effective serotonin precursor. Alternative Medicine Review: A Journal of Clinical Therapeutic, 3(4), 271-280. https://pubmed.ncbi.nlm.nih.gov/9727088/
- Okawa, M., Uchiyama, M., Ozaki, S., Shibui, K., & Ichikawa, H. (1997). Circadian rhythm sleep disorders in adolescents: clinical trials of combined treatments based on chronobiology. Psychiatry and Clinical Neurosciences, 51(5), 333-339. https://pubmed.ncbi.nlm.nih.gov/10215009/
- McCarty, D. E., Chesson Jr, A. L., Jain, S. K., & Marino, A. A. (2012). The link between vitamin D metabolism and sleep medicine. Sleep Medicine Reviews, 18(4), 311-319. https://pubmed.ncbi.nlm.nih.gov/24075129/
- Abbasi, B., Kimiagar, M., Sadeghniiat, K., Shirazi, M. M., Hedayati, M., & Rashidkhani, B. (2012). The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences, 17(12), 1161–1169. https://pubmed.ncbi.nlm.nih.gov/23853635/
- Kerley, C. P., Hutchinson, K., Bolger, K., McGowan, A., Faul, J., & Cormican, L. (2020). Serum vitamin D is significantly inversely associated with disease severity in Caucasian adults with obstructive sleep apnea syndrome. Sleep, 39(2), 293-300. https://pubmed.ncbi.nlm.nih.gov/26414899/
- Montgomery, P., Burton, J. R., Sewell, R. P., Spreckelsen, T. F., & Richardson, A. J. (2014). Fatty acids and sleep in UK children: subjective and pilot objective sleep results from the DOLAB study–a randomized controlled trial. Journal of Sleep Research, 23(4), 364–388. https://pubmed.ncbi.nlm.nih.gov/24605819/
- Hartmann, E. (1982). Effects of L-tryptophan on sleepiness and on sleep. Journal of Psychiatric Research, 17(2), 107-113. https://pubmed.ncbi.nlm.nih.gov/6764927/
- Lavie, L., Lavie, P. (2009). Molecular mechanisms of cardiovascular disease in OSAHS: the oxidative stress link. European Respiratory Journal, 33(6), 1467-1484. https://erj.ersjournals.com/content/33/6/1467
- Tan, K. C., Chow, W. S., Lam, J. C., Lam, B., Bucala, R., Betteridge, J., & Ip, M. S. (2013). Advanced glycation endproducts in nondiabetic patients with obstructive sleep apnea. Sleep, 36(3), 399–403 https://academic.oup.com/sleep/article/29/3/329/2708065
- Gozal, D., Kheirandish-Gozal, L., Bhattacharjee, R., & Molero-Ramirez, H. (2013). Circulating adropin concentrations in pediatric obstructive sleep apnea: potential relevance to endothelial function. Journal of Pediatrics, 163(4), 1122-1126. https://pubmed.ncbi.nlm.nih.gov/23810721/
- Miller, E. R., Pastor-Barriuso, R., Dalal, D., Riemersma, R. A., Appel, L. J., & Guallar, E. (2005). Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Annals of internal medicine, 142(1), 37–46. https://pubmed.ncbi.nlm.nih.gov/15537682/
- Klein, E. A., Thompson, I. M., Tangen, C. M., Crowley, J. J., Lucia, M. S., Goodman, P. J., Minasian, L. M., Ford, L. G., Parnes, H. L., Gaziano, J. M., Karp, D. D., Lieber, M. M., Walther, P. J., Klotz, L., Parsons, J. K., Chin, J. L., Darke, A. K., Lippman, S. M., Goodman, G. E., … Baker, L. H. (2011). Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA, 306(14), 1549–1556. https://pubmed.ncbi.nlm.nih.gov/21990298/
- Lobo, V., Patil, A., Phatak, A., & Chandra, N. (2010). Free radicals, antioxidants and functional foods: Impact on human health. Pharmacognosy Reviews, 4(8), 118–126. https://pubmed.ncbi.nlm.nih.gov/22228951/
- Bjelakovic, G., Nikolova, D., Gluud, L. L., Simonetti, R. G., & Gluud, C. (2014). Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane Database of Systematic Reviews, (3). https://pubmed.ncbi.nlm.nih.gov/22419320/
- Frank, L.L. (2019). Thiamine in Clinical Practice. JPEN Journal of Parenteral and Enteral Nutrition, 39(5), 503–520. https://pubmed.ncbi.nlm.nih.gov/25564426/
- Tamura, T., & Picciano, M. F. (2006). Folate and human reproduction. The American Journal of Clinical Nutrition, 83(5), 993–1016. https://pubmed.ncbi.nlm.nih.gov/16685040/
- Lemoine, P., Nir, T., Laudon, M., & Zisapel, N. (2007). Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. Journal of sleep research, 16(4), 372–380. https://pubmed.ncbi.nlm.nih.gov/18036082/
- Andersen, L. P., Gögenur, I., Rosenberg, J., & Reiter, R. J. (2016). The Safety of Melatonin in Humans. Clinical Drug Investigation, 36(3), 169–175. https://pubmed.ncbi.nlm.nih.gov/26692007/
- Auld, F., Maschauer, E. L., Morrison, I., Skene, D. J., & Riha, R. L. (2017). Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders. Sleep Medicine Reviews, 34, 10–22. https://pubmed.ncbi.nlm.nih.gov/28648359/
- Srinivasan, V., Singh, J., Pandi-Perumal, S. R., Brown, G. M., Spence, D. W., & Cardinali, D. P. (2011). Jet lag, circadian rhythm sleep disturbances, and depression: the role of melatonin and its analogs. Advances in Therapy, 27(11), 796–813. https://pubmed.ncbi.nlm.nih.gov/20827520/