Obstructive Sleep Apnea Pulse Pressure

Obstructive sleep apnea (OSA) and heart problems such as hypertension (also known as ‘high blood pressure’) are commonly associated with each other. It’s not unusual for a person to experience both health issues at the same time.
Numerous studies identified OSA as a contributor to the development of hypertension. As such, OSA patients should diligently manage their hypertension as part of their approach to managing sleep apnea.
Many patients with OSA use daily trackers like an Oura Ring or Fitbit for sleep to check important vitals such as heart rate, blood pressure, and sleep patterns as part of their daily health routines.
How Obstructive Sleep Apnea Affects the Heart
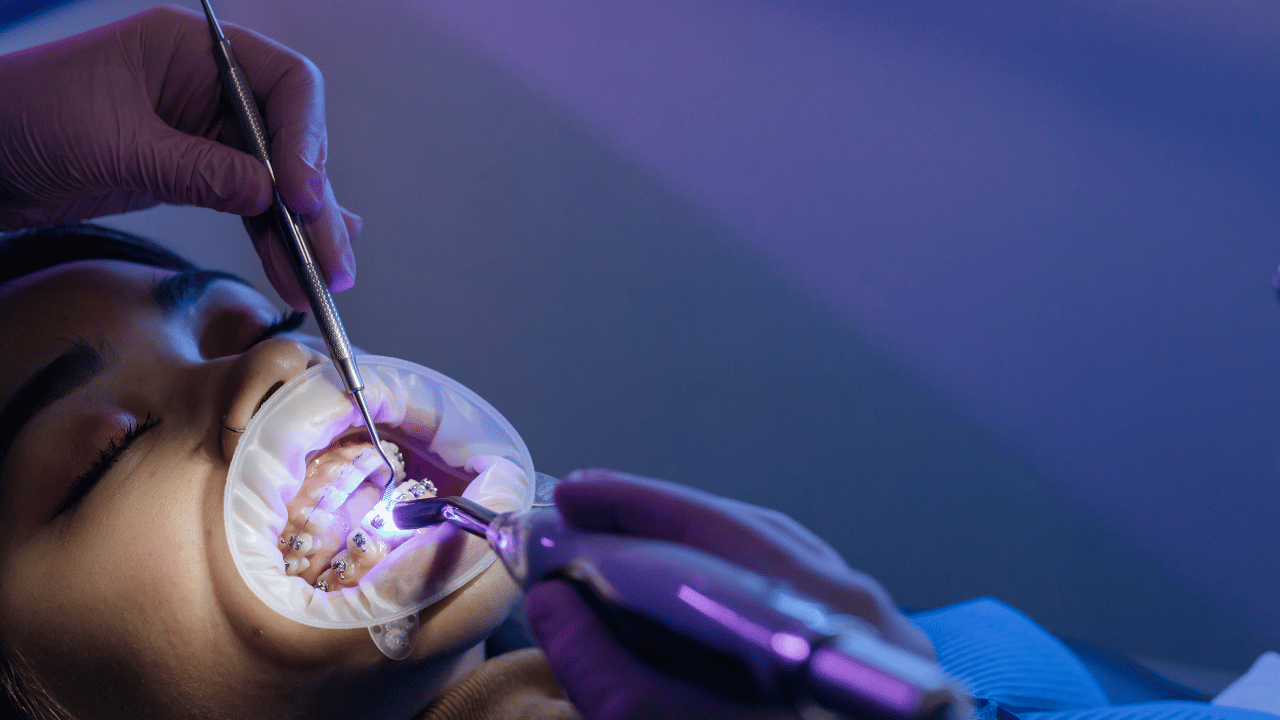
After your health practitioner walks you through how to read sleep apnea test results and concludes that you have OSA, it’s important to pay close attention to your symptoms and the possible complications. Sleep is an important lifestyle factor that can impact your body (particularly your heart) in many ways.
For example, OSA can lead to a variety of heart conditions, including atrial fibrillation (irregular heartbeat), coronary artery disease (hardened arteries), and bradycardia (slow heart rate). One of the most common cardiovascular issues in OSA patients is hypertension. Numerous studies suggest a sleep disorder like OSA is an independent risk factor for hypertension.
According to the American Thoracic Society, about 30% of hypertensive patients suffer from OSA. There is also a 50% chance that you have hypertension if you have OSA. One study showed that OSA is associated with an increased future risk of hypertension independent of age, sex, body mass index, and other demographics.
It is believed that the link between OSA and hypertension is due to the disruptive breathing patterns typical of sleep apnea causing stress to the heart. When you take prolonged gaps between breaths, you decrease the level of oxygen in your blood. This signals your heart to beat faster, elevating your blood pressure. Some patients are encouraged to use devices such as a sleep apnea oxygen concentrator to better control blood oxygen concentration and help ease hypertension.

Managing Hypertension in OSA Patients
The connection between OSA and hypertension highlights the importance of managing sleep apnea symptoms to decrease their potential adverse effect on the heart. There are several methods to deal with OSA, with continuous positive airway pressure (CPAP) generally being the first-line approach.
That said, dependence on CPAP devices is not an option for many OSA patients. Additionally, it only delivers a modest reduction in blood pressure. As such, many health practitioners rely on pharmacological therapy to control blood pressure, but data is limited on the efficacy of these drugs in patients aiming to control hypertension as a complication of OSA.
Fortunately, there are natural ways to deal with sleep apnea, including promoting proper breathing, losing weight, and setting up sleep-conducive environments.
Overcoming Sleep Apnea
Sleep apnea can significantly impact your life because it affects how your body performs day-to-day. If you’re looking for alternatives to CPAP or are hoping to follow a different method to enhance natural sleep, you can find our book Sleep Apnea Solution on Amazon. It includes helpful guides and natural approaches for addressing sleep apnea symptoms!